Beyond Condoms: Exploring Additional Measures for STD Prevention and Control
Beyond Condoms: Exploring Additional Measures for STD Prevention and Control
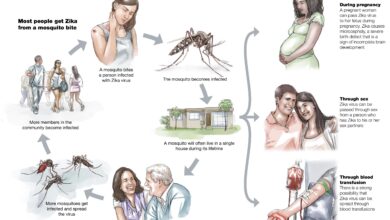
Sexually transmitted diseases (STDs) remain a significant public health concern globally, with millions of new cases reported each year. While condoms have long been promoted as a primary method of prevention, it’s crucial to recognize that they aren’t foolproof. In this article, we’ll delve into additional measures for STD prevention and control, considering the diverse strategies and interventions available to mitigate the spread of these infections.
The Limitations of Condoms
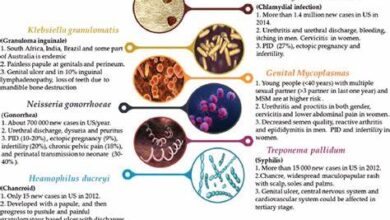
Condoms are undoubtedly an essential tool in preventing the transmission of STDs, including HIV, gonorrhea, chlamydia, and syphilis. However, their effectiveness relies heavily on consistent and correct usage, which may not always be achievable due to various factors such as lack of access, reluctance, or human error. Moreover, condoms may not provide complete protection against certain infections like herpes and human papillomavirus (HPV), as they can be transmitted through skin-to-skin contact in areas not covered by the condom.
Comprehensive Sex Education
One of the most effective long-term strategies for STD prevention is comprehensive sex education. Providing accurate, age-appropriate information about sexual health, consent, contraception, and STD prevention empowers individuals to make informed decisions about their bodies and relationships. Comprehensive sex education also addresses myths and misconceptions surrounding STDs, reduces stigma, and encourages open communication about sexual health issues.
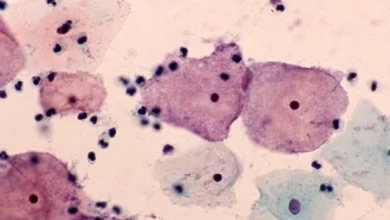
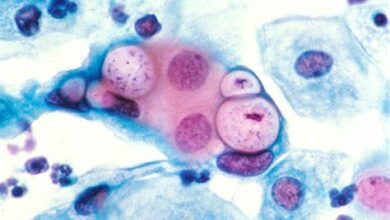
Routine Screening and Testing
Regular screening and testing for STDs are vital components of prevention and control efforts. Early detection allows for timely treatment, reducing the risk of complications and further transmission. Healthcare providers recommend routine screening for STDs, especially among sexually active individuals, pregnant women, and those at higher risk due to multiple sexual partners or engaging in unprotected sex. Testing should encompass a broad range of infections, including HIV, syphilis, gonorrhea, chlamydia, and hepatitis B and C.
Pre-Exposure Prophylaxis (PrEP) and Post-Exposure Prophylaxis (PEP)
Pre-exposure prophylaxis (PrEP) involves taking antiretroviral medication regularly to prevent HIV infection in individuals at high risk, such as those with an HIV-positive partner or those engaging in behaviors that increase their vulnerability. Similarly, post-exposure prophylaxis (PEP) involves taking antiretroviral drugs within 72 hours of potential HIV exposure to reduce the risk of infection. Both PrEP and PEP have shown to be highly effective in preventing HIV transmission when used correctly and consistently.
Vaccination Against STDs
Vaccination represents a groundbreaking approach to STD prevention, particularly for viral infections like HPV and hepatitis B. The HPV vaccine, available for both males and females, protects against several strains of the virus responsible for cervical, anal, and oropharyngeal cancers, as well as genital warts. Similarly, the hepatitis B vaccine offers long-term protection against a virus that can cause liver disease and cancer. By increasing vaccine uptake, especially among adolescents and young adults, we can significantly reduce the burden of these preventable infections.
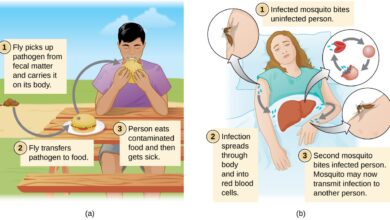
Addressing Socioeconomic and Structural Factors
It’s essential to recognize that STD risk is influenced by socioeconomic and structural factors such as poverty, lack of access to healthcare, discrimination, and stigma. To effectively combat STDs, interventions must address these underlying determinants of health. This includes expanding access to affordable healthcare services, promoting equity in sexual health education and resources, and addressing societal attitudes and norms that contribute to stigma and discrimination against marginalized populations.
Conclusion
While condoms remain a cornerstone of STD prevention, it’s evident that a comprehensive approach is necessary to address the complex challenges posed by these infections. By combining multiple strategies, including comprehensive sex education, routine screening, pre-exposure and post-exposure prophylaxis, vaccination, and addressing socioeconomic and structural factors, we can create a more resilient and effective framework for STD prevention and control. It’s imperative that policymakers, healthcare providers, educators, and communities work together to implement evidence-based interventions and reduce the burden of STDs on individuals and society as a whole.
- Baby names starting with A
- Baby names starting with B
- Baby names starting with C
- Baby names starting with D
- Baby names starting with E
- Baby names starting with F
- Baby names starting with G
- Baby names starting with H
- Baby names starting with I
- Baby names starting with J
- Baby names starting with K
- Baby names starting with L
- Baby names starting with M
- Baby names starting with N
- Baby names starting with O
- Baby names starting with P
- Baby names starting with Q
- Baby names starting with R
- Baby names starting with S
- Baby names starting with T
- Baby names starting with U
- Baby names starting with V
- Baby names starting with W
- Baby names starting with X
- Baby names starting with Y
- Baby names starting with Z